Want to find out more about any of the above services?
We’d like to hear from you, click below to get in
touch with our experienced sales team!
Coverage Viewer Tool
The Coverage Viewer Tool utilizes Policy Reporter’s proprietary Payer policy tracking software to provide an easy-to-use and powerful lookup tool for coverage, criteria and restrictions across Payers. Our interactive dashboard allows you to drill down by region, Payer, and plan or view national and regional coverage criteria, and statistics of your drug, device, or therapy.
Common Uses of the Payer Coverage Summary Tool
Your sales team may use the Coverage Summary Tool to identify, assess and optimize patient access for select drugs of interest. Policy Reporter’s Payer Coverage Summary Tool is designed so that each of your account managers can strategically focus their sales efforts, and inform physicians of the latest criteria.
By utilizing the Payer Coverage Summary Tool, you can quickly view, monitor, and analyze coverage for your drug, and competitor drugs, instantly across all 50 states, enabling you to effectively strategize and ensure commercial success.
Our Clients Use This Tool To:
Empower Your Teams
The Payer Coverage Summary Tool is a valuable resource in the field. Your sales team can log in and strategically plan their provider visits and can quickly assess what market access opportunities there are for your drug, device, test, or therapy by each Payer in their assigned territory or state.
By providing your team with this tool, they can look up payers and coverage criteria as needed, saving valuable time and resources.
Inform Your Providers
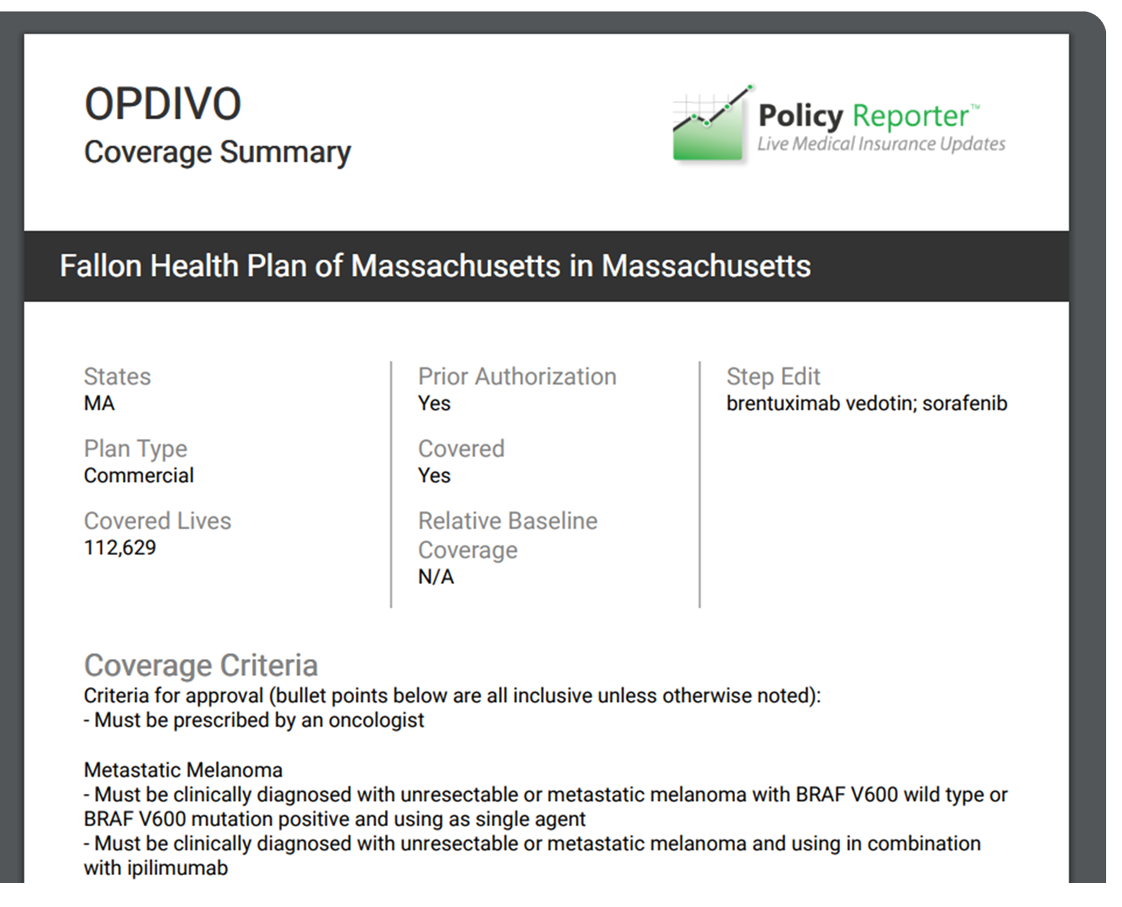
Using this tool, your team can export either a simplified or detailed summary of coverage criteria as a useful leave-behind for providers.
At each provider meeting, your account manager can bring this summarized export, which highlights coverage by plan for your drug, and indicates criteria and prior authorization steps.
This leave-behind document can be branded and customized to your company’s standards, and serves as a succinct and powerful reminder of what was discussed during the meeting while outlining the treatment, coverage criteria, and authorization requirement for your product.